Is a home insemination kit actually worth trying before IVF? When should you do ICI so you don’t waste a cycle? And what are people talking about right now—legally and culturally—around at-home fertility?

Yes, a home insemination kit can be a practical first step for some families. Timing is the make-or-break factor, not “doing more.” And the conversation is loud right now: court decisions, ongoing reproductive-rights litigation, and nonstop fertility chatter in media all shape how people plan.
Overview: What ICI at home is (and what it isn’t)
ICI stands for intracervical insemination. It’s a method where semen is placed near the cervix using a syringe, typically after tracking ovulation. People consider ICI for many reasons: budget, privacy, LGBTQ+ family building, single parents by choice, or as a step before clinical options.
ICI is not IVF. It also isn’t a medical procedure in the same way IUI is (intrauterine insemination), where sperm is placed in the uterus by a clinician. With ICI, your main levers are timing, comfort, and using clean, appropriate supplies.
Culture-wise, it’s hard to miss the current wave of fertility conversations—from “age 35” debates to TV-drama storylines where couples face setbacks and keep going. That mix of hope and uncertainty is real. Planning helps turn that noise into a calmer next step.
Timing: The cycle window that matters most
If you only optimize one thing, make it timing. Many “it didn’t work” cycles come down to inseminating too early or too late.
Pick a tracking method you can stick with
Choose one primary method and use it consistently for a full cycle or two:
- Ovulation predictor kits (OPKs): Look for an LH surge. Ovulation often follows within roughly a day or two.
- Cervical mucus changes: Many people notice more clear, stretchy mucus near ovulation.
- Basal body temperature (BBT): Confirms ovulation after it happens, which is helpful for learning patterns.
Apps can help you log, but predictions are not the same as your body’s signals. If you’re curious about how tools “guess” fertile days, a lot of modern health tech leans on pattern recognition. If you want a plain-language explainer, see home insemination kit.
A simple timing approach that avoids overdoing it
To stay budget-friendly, aim for attempts centered on your strongest fertility signs. Many people try once around the positive OPK and once again the next day. If you’re using mucus tracking, focus on the day(s) with the most fertile-quality mucus and the day after.
If cycles are irregular, consider tracking longer before you spend money on repeated attempts. That alone can prevent “we tried but missed it” frustration.
Supplies: What you need (and what to skip)
Keep it simple. A good setup is about the right items, not a long shopping list.
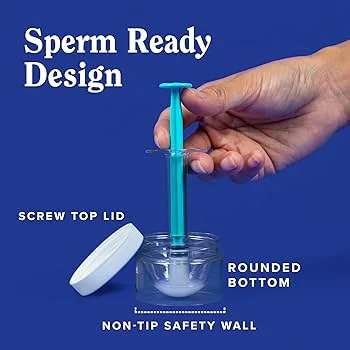
- Syringes designed for insemination (no needles). A rounded tip is often more comfortable.
- Collection container if using fresh semen.
- Optional: fertility-friendly lubricant (only if needed).
- Clean, comfortable space and a timer/clock.
Skip anything that adds irritation or contamination risk. Avoid scented products. Don’t use random household applicators. If you’re looking for a purpose-built option, see this at-home insemination kit for ICI.
Step-by-step: A practical ICI routine at home
This is a general overview for educational purposes. Follow product instructions and prioritize comfort.
1) Set up before you start
Wash hands. Lay out supplies. Give yourselves time so it doesn’t feel rushed. Stress doesn’t “ruin” a cycle, but rushing can create avoidable mistakes.
2) Collect and prepare
If using fresh semen, collect into a clean container. Let it liquefy for a short period if needed so it draws into the syringe more easily. Keep everything at room temperature unless you’ve been instructed otherwise by a licensed professional.
3) Draw into the syringe gently
Pull the plunger back slowly to reduce bubbles. If you see large air pockets, pause and adjust. You’re aiming for a smooth, controlled delivery.
4) Insert and inseminate slowly
Find a comfortable position. Insert the syringe only as far as it comfortably goes (ICI stays near the cervix; force is never the goal). Depress the plunger slowly. Then remove the syringe gently.
5) Rest briefly, then move on with your day
Many people rest for 10–20 minutes. Some elevate hips; others don’t. Choose what feels calming, not what feels like a performance.
Mistakes that waste a cycle (and how to avoid them)
- Mistiming the attempt: Don’t rely on app guesswork alone. Use OPKs and/or body signs.
- Trying too many times: More attempts can mean more cost and more pressure. Focus on the best days.
- Using the wrong lubricant: Some lubes are not sperm-friendly. If you need lube, choose a fertility-friendly option.
- Rough technique: Discomfort can make it harder to repeat next cycle. Slow and gentle wins.
- Ignoring the legal side with a known donor: Headlines have highlighted that at-home donor arrangements can create unexpected parentage outcomes in some places. Get local legal advice before you begin.
On that last point: reproductive-rights policy and court cases are changing and contested. Ongoing litigation in federal courts keeps the topic in motion. If you’re building a family with a donor, treat legal planning as part of your “supplies.”
FAQ: Quick answers before you try
Is ICI painful?
It shouldn’t be. Mild discomfort can happen, but pain is a sign to stop and reassess technique or supplies.
How long should I rest after insemination?
Many people choose 10–20 minutes. The goal is comfort and calm, not a perfect ritual.
What if I’m 35+ and worried about a “fertility cliff”?
Age-related fertility changes are real, but the timeline isn’t identical for everyone. If you’re concerned, consider getting basic fertility testing through a clinician while you plan next steps.
When should we consider moving from ICI to clinical options?
If you’ve tried several well-timed cycles without success, or if you already know there are factors like blocked tubes or severe sperm issues, talk with a fertility clinician about IUI/IVF.
Medical disclaimer: This article is educational and not medical advice. It does not diagnose, treat, or replace care from a licensed clinician. If you have pelvic pain, a history of infection, known fertility conditions, or questions about donor arrangements, consult a qualified healthcare professional and, when relevant, a family law attorney in your area.
Next step: Make your first ICI attempt more predictable
If you want a simple setup that supports a calmer, less wasteful try, start with the right supplies and a timing plan you can repeat next cycle.