- ICI is a real option when you want privacy, lower costs, and more control than clinic-based treatment.
- Safety isn’t just about cleanliness; it also includes screening, consent, and documentation.
- Timing matters more than gadgets; a simple plan around ovulation beats guesswork.
- Supplements are trending, but evidence varies—don’t let marketing replace basics like timing and health review.
- Legal and access issues are in the news; plan ahead so your family-building choices stay protected.
Big picture: why at-home insemination is getting so much attention
Pop culture has a way of making pregnancy feel like a constant headline. Between celebrity baby announcements and the usual swirl of “who’s expecting” chatter, it’s easy to forget that many people are quietly trying for months or years. That contrast is one reason at-home insemination (ICI) keeps coming up in conversations.

At the same time, fertility products and supplements are being discussed more broadly, including market reports that highlight how fast the category is growing. Add ongoing debates about reproductive healthcare access and court cases, and you get a climate where people want options that feel private, practical, and within reach.
ICI (intracervical insemination) is often discussed as a home fertility option and, for some, an IVF alternative. It’s not a perfect substitute for medical care. Still, it can be a meaningful first step for certain couples and solo parents, especially when there are no known infertility diagnoses.
The emotional side: privacy, pressure, and “headline culture”
Celebrity pregnancies can be fun to follow, but they can also sting. You might feel behind, isolated, or rushed. Those feelings are normal, and they can push people into decisions that aren’t fully thought through.
Try to separate the story you see from the story you’re living. A calm plan helps. So does choosing an approach that fits your values: privacy, budget, medical involvement, or legal clarity.
If you’re doing ICI with a partner, talk about what success and “pause” look like before you start. If you’re using a donor, talk about boundaries and expectations early, not mid-cycle.
Practical steps: a simple ICI plan you can actually follow
1) Decide what “at-home” means for you
At-home insemination can range from fully DIY to a hybrid approach where a clinician helps with testing, cycle monitoring, or preconception labs. Your plan can be private without being unsupported.
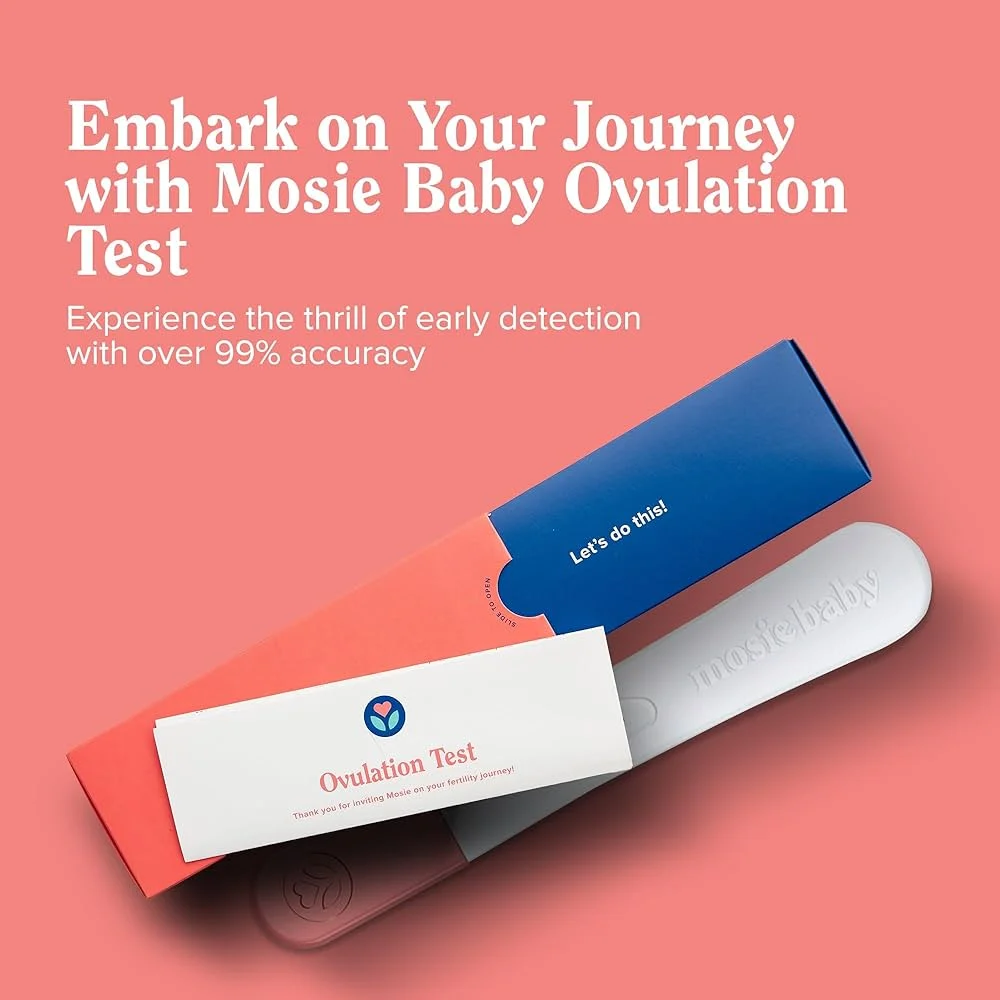
2) Track ovulation with a two-signal approach
Don’t rely on a single clue. Many people combine:
- Ovulation predictor kits (LH tests) to spot the surge
- Cervical mucus changes (more slippery/egg-white-like near the fertile window)
If your cycles are irregular, consider adding basal body temperature tracking or asking a clinician about monitoring. A little structure can save months of mistimed attempts.
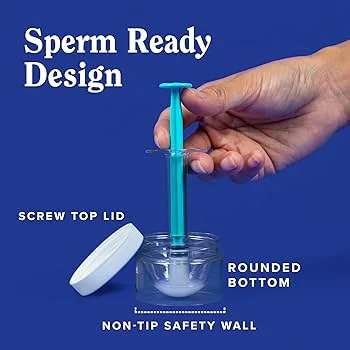
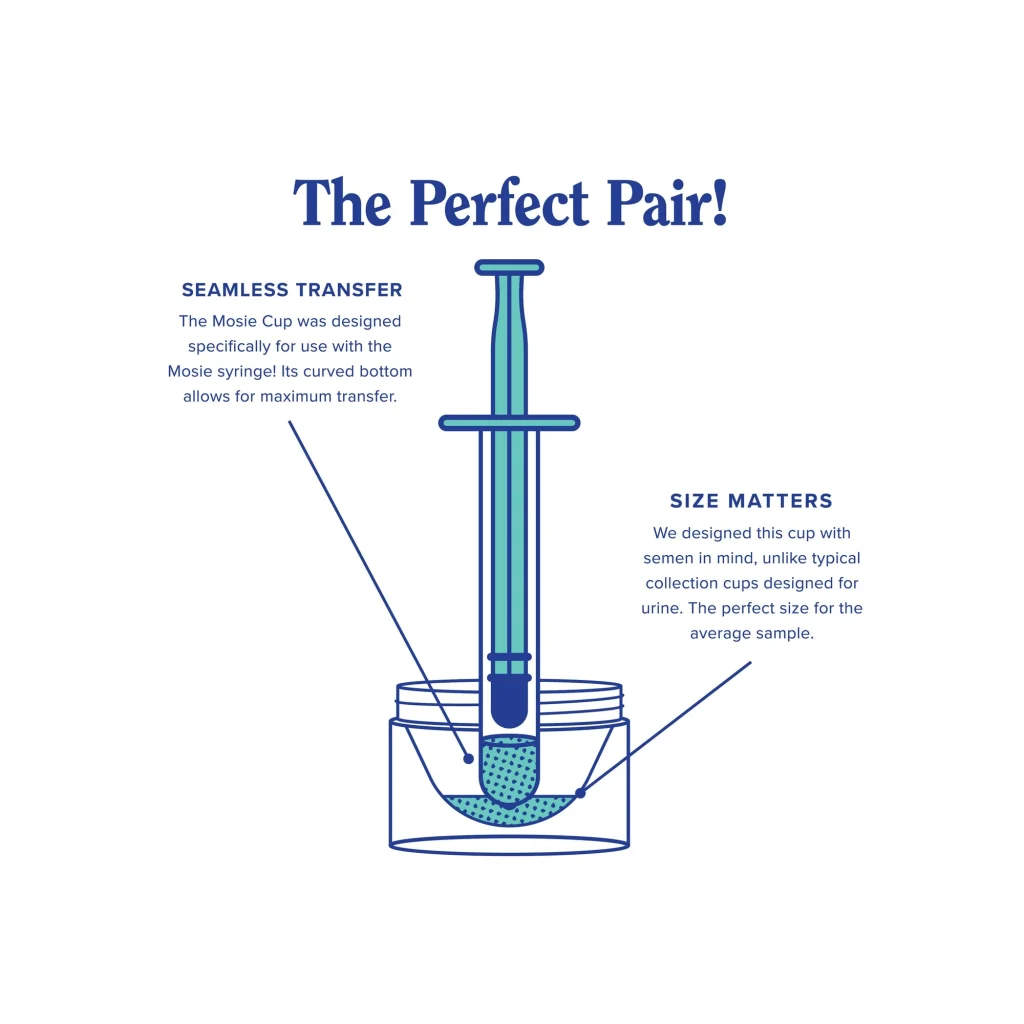
3) Choose supplies that reduce mess and guesswork
A home insemination kit is meant to make the process more consistent: controlled transfer, less spillage, and fewer improvised tools. You’re aiming for repeatable steps, not a “perfect” setup.
If you’re looking for a dedicated option, consider a at-home insemination kit for ICI that’s designed for this use case rather than repurposed items.
4) Create a short, written cycle log
Keep a note on your phone with:
- Cycle day and LH test results
- Insemination date/time
- Any symptoms (cramping, spotting, stress, illness)
This is useful for you, and it’s also helpful if you later consult a clinician. It turns “we tried a lot” into information that can guide next steps.
Safety and testing: reduce infection, legal, and documentation risks
Clean technique and realistic hygiene
Use clean hands, clean surfaces, and single-use components when applicable. Avoid unapproved lubricants and avoid inserting anything not intended for vaginal use. If you have pain, fever, or unusual discharge after an attempt, seek medical care promptly.
Screening: think in layers, not loopholes
When people talk about “safe,” they often mean “I won’t get an infection.” That matters, but it’s only one layer. Consider:
- STI testing for involved partners/donors (timed appropriately)
- Health history review and genetic considerations (as relevant)
- Specimen handling and storage practices, especially with shipped or frozen samples
Testing choices depend on your location, your risk tolerance, and how you’re sourcing sperm. When in doubt, ask a clinician or a reputable testing provider for guidance.
Legal clarity: don’t skip the unglamorous part
Reproductive health and rights are frequently debated in policy and the courts, and the practical takeaway is simple: rules can be complicated and they can change. If donor arrangements or parentage could ever be questioned, get qualified legal advice.
Many families reduce risk by documenting consent, expectations, and parentage intentions in writing. A local attorney who works in reproductive or family law is the best source here.
Digital tools and privacy
Some people use apps to track cycles, symptoms, or timing predictions. Others prefer a paper log. If you use tech tools, review privacy settings and consider what you share.
You’ll also see more fertility tools marketed as “smart” or “AI-powered.” If you want context on the term itself, see home insemination kit. Even with advanced predictions, your body’s signals still matter most.
Supplements and “what people are buying right now”
Fertility supplements are having a moment, and market coverage reflects that. Some supplements may be appropriate for specific deficiencies, but the evidence is mixed across products and people. Don’t let a trend replace fundamentals like timing, screening, and medical review when needed.
If you’re considering supplements, it’s reasonable to run them by a clinician or pharmacist—especially if you take other medications or have thyroid, PCOS, or metabolic concerns.
Medical disclaimer
This article is for general educational information and does not provide medical advice, diagnosis, or treatment. Fertility needs are personal. For guidance on testing, medications, infection symptoms, or underlying conditions, consult a licensed healthcare professional.
Next step: get a clear, safer plan for this cycle
If you want a private approach with more structure, start with a kit designed for ICI and a short checklist for timing, screening, and documentation. The goal is not perfection. It’s a repeatable process you can feel good about.