Is a home insemination kit actually worth trying?
When should you time ICI so you’re not guessing?
And what do you need to do to reduce infection and legal risk?

Those are the three questions people keep asking—especially when celebrity pregnancy news is everywhere and timelines feel loud. Add recent headlines about a Florida court decision involving at-home insemination, and it’s no surprise more people are looking for clear, practical answers. This guide walks through ICI (intracervical insemination) at home in a grounded way: timing, supplies, steps, common mistakes, and the “paperwork” mindset that can protect you later.
Medical disclaimer: This article is educational and not medical or legal advice. It can’t diagnose conditions or replace care from a licensed clinician or attorney. If you have urgent symptoms, seek medical care.
The big picture: ICI at home as a fertility option
ICI is a method where sperm is placed near the cervix around ovulation. It’s often discussed as a lower-intervention option compared with clinic-based treatments. Some people explore it as an IVF alternative, while others see it as a first step before moving to a fertility clinic.
What’s driving the conversation right now isn’t just pop culture baby buzz. Legal headlines have also pushed people to ask: “If we do this at home with a known donor, what could happen later?” Keep that question in your plan from day one.
Timing that makes sense (without turning your life into a spreadsheet)
ICI is timing-sensitive. If you miss the fertile window, perfect technique won’t matter much. The goal is to inseminate close to ovulation, when cervical mucus is more sperm-friendly.
Use two signals, not one
Most people rely on a combination of:
- Ovulation predictor kits (OPKs): Look for an LH surge.
- Cervical mucus changes: Often becomes clearer, stretchy, and slippery near ovulation.
If you only use calendar math, irregular cycles can throw you off. If you only use symptoms, stress and illness can blur the picture. Two signals reduce guesswork.
A practical timing target
Many try ICI the day they see a positive OPK and again the next day. Your body may differ. If your cycles are unpredictable, consider tracking for a few months before you invest time and emotion into a single attempt.
Supplies checklist: what to gather (and what to skip)
At-home insemination works best when you treat it like a clean, planned process. That means using appropriate supplies and avoiding “DIY shortcuts” that can irritate tissue.
Basic items many people use
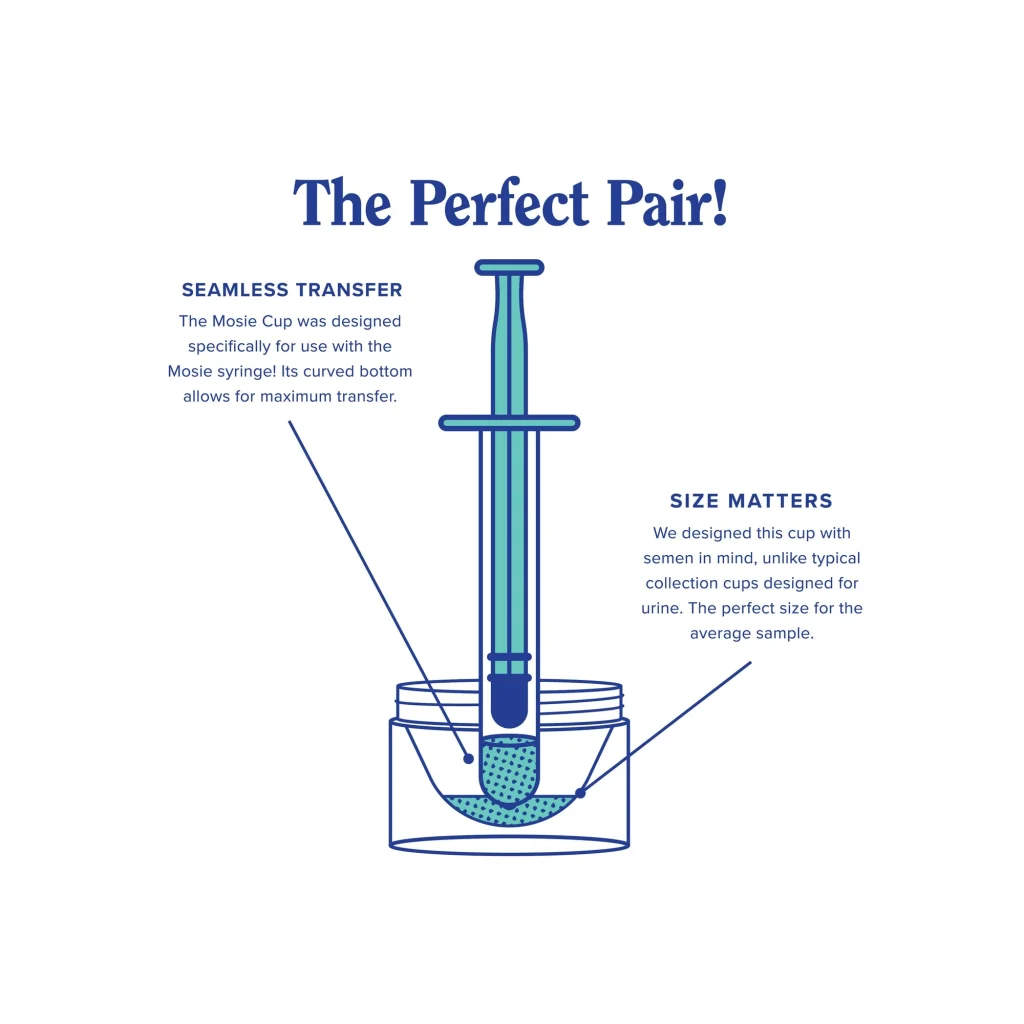
- Home insemination kit with a needle-free syringe designed for this purpose
- Single-use collection container (if collecting at home)
- Clean towels or disposable pads
- Water-based lubricant (optional; avoid sperm-toxic lubes)
- OPKs and a simple tracking method (app or notes)
Skip these common “bad ideas”
- Reusing syringes or containers
- Using random household tools that aren’t designed for body-safe use
- Harsh soaps or douching (can irritate and disrupt the vaginal environment)
Step-by-step: an ICI routine you can follow at home
This is a general, non-clinical overview. Always follow the instructions that come with your kit. If you’re using donor sperm from a bank or working with a clinic, follow their handling rules closely.
1) Set up a calm, clean space
Wash hands well. Lay out supplies so you’re not scrambling mid-process. Stress doesn’t “ruin” ICI, but rushing can lead to spills, contamination, or forgotten steps.
2) Confirm your timing
Use your OPK result and your body signs. If you’re not near the fertile window, it’s usually better to wait than to force an attempt “just in case.”
3) Collect and load carefully
Follow your kit’s directions for collection and drawing into the syringe. Keep everything as clean as possible. Avoid introducing air bubbles if your instructions advise against it.
4) Place sperm at the cervix (ICI)
Get into a comfortable position. Insert only as far as the instructions indicate. Then dispense slowly. Fast pressure can cause discomfort and increases the chance of leakage.
5) Rest briefly, then return to normal
Many people choose to lie down for 10–20 minutes. Do what feels comfortable. After that, normal movement is fine.
6) Document what you did
Write down the date, OPK result, and any notes (timing, mucus, any discomfort). If you’re using a known donor, documentation can also include what was agreed to and how it was handled.
Mistakes that waste the window (or create avoidable risk)
People often focus on the syringe and forget the bigger system: timing, screening, and clarity. Here are the pitfalls that come up most.
Missing the fertile window
Trying too early or too late is the #1 issue. If you can only do one attempt, prioritize the surge day and shortly after.
Ignoring infection and screening basics
If you’re working with a known donor, talk about STI testing and timelines. This is a health decision, not a vibe check. If you’re unsure what to request, a clinician can help you understand general screening options.
Using informal donor arrangements without legal clarity
Recent reporting has highlighted court disputes where at-home insemination didn’t automatically eliminate parental rights. That doesn’t mean every arrangement leads to conflict. It does mean you should treat the legal side as real, even if everyone is friendly today.
If you want to read more about the general news coverage that sparked this conversation, see: Florida Supreme Court makes ruling in at-home artificial insemination case.
Chasing “celebrity timeline” expectations
Celebrity pregnancy announcements can make it feel like everyone gets a happy update on schedule. Real life is messier. Give yourself a plan that includes emotional pacing, not just logistics.
FAQ: quick answers people want before they try ICI
Is a home insemination kit safe?
It can be safer when you use single-use, body-safe supplies and keep things clean. Screening and proper handling matter too. If you have pain, fever, or unusual discharge after attempting insemination, seek medical care.
How many tries should I do before changing plans?
That depends on age, cycle regularity, and known fertility factors. If you’ve tried multiple well-timed cycles without success, a clinician can help you decide whether testing, IUI, or IVF makes sense.
Does orgasm, position, or a pillow matter?
Comfort matters more than “hacks.” There isn’t one proven position that guarantees success. Focus on timing and clean technique.
CTA: choose a kit that supports clean, controlled ICI
If you’re ready to plan your attempt, start with supplies designed for this purpose. A purpose-built at-home insemination kit for ICI can help you avoid improvising and keep the process straightforward.
How does at-home insemination (ICI) work?
One more smart step: if you’re using a known donor, consider getting state-specific legal advice before you try. Clear agreements and documentation can prevent future conflict and protect everyone involved.