Before you try at-home insemination, check these boxes:

- Timing: You have a plan to identify your fertile window (not just a guess).
- Tools: You know what’s in your home insemination kit and what you will not do at home.
- Consent: Everyone involved is clear on boundaries and expectations.
- Legal reality: You’ve considered parentage rules where you live—especially if a donor is involved.
- Emotional bandwidth: You’ve talked about how you’ll handle a negative test, a delay, or a change of plan.
Right now, a lot of people are talking about at-home fertility options the way they talk about a buzzy TV plotline: private choices, big consequences, and a surprise twist from the courts. Recent reporting out of Florida has pushed one specific issue into the spotlight—whether an at-home donor can later seek legal parent status. If you’re considering ICI, it’s a reminder to plan for more than just ovulation.
Decision guide: If this is your situation, then consider this
If you want the most privacy, then keep it simple—and document your decisions
At-home ICI appeals because it can feel calmer than clinics. It also gives you control over who’s in the room and how the process looks. That privacy can reduce stress, but it can also create gaps: fewer witnesses, fewer records, and more room for misunderstandings later.
If you’re using a known donor, treat clarity like a safety tool. Write down expectations, communication rules, and what “involvement” means. Then get legal advice before any attempt, not after a positive test.
If you’re using a known donor, then assume parentage questions may come up
Some recent Florida coverage suggests that at-home donors may be able to ask courts to recognize them as legal parents in certain circumstances. The details can vary by case and by state, but the theme is consistent: at-home insemination can land in family court if expectations aren’t aligned.
For a general reference point, you can review related coverage by searching this topic here: Florida Supreme Court makes ruling in at-home artificial insemination case.
If cost is the pressure point, then compare ICI vs IVF without shame
Money stress changes relationships fast. Many couples and solo parents weigh ICI because IVF can feel financially out of reach. That reality shows up in conversations across the internet, including LGBTQ+ families who worry that the path to parenthood will cost more than they can sustain.
Here’s the practical move: list your options as “next steps,” not forever decisions. You can try ICI for a defined number of cycles, then reassess. A time-boxed plan often reduces conflict because it replaces endless debating with a shared checkpoint.
If you’re overwhelmed by headlines, then focus on the parts you control this week
Reproductive-health news cycles can feel relentless. Court updates, state-by-state policy changes, and social media hot takes can make a personal decision feel political overnight. If you notice that spiral, narrow your scope.
- Pick one tracking method you can stick with.
- Choose a kit that matches ICI (not clinic-only procedures).
- Schedule one legal consult if a donor is involved.
- Agree on one communication rule (for example: no “post-test blame” talk).
What a home insemination kit is (and what it isn’t)
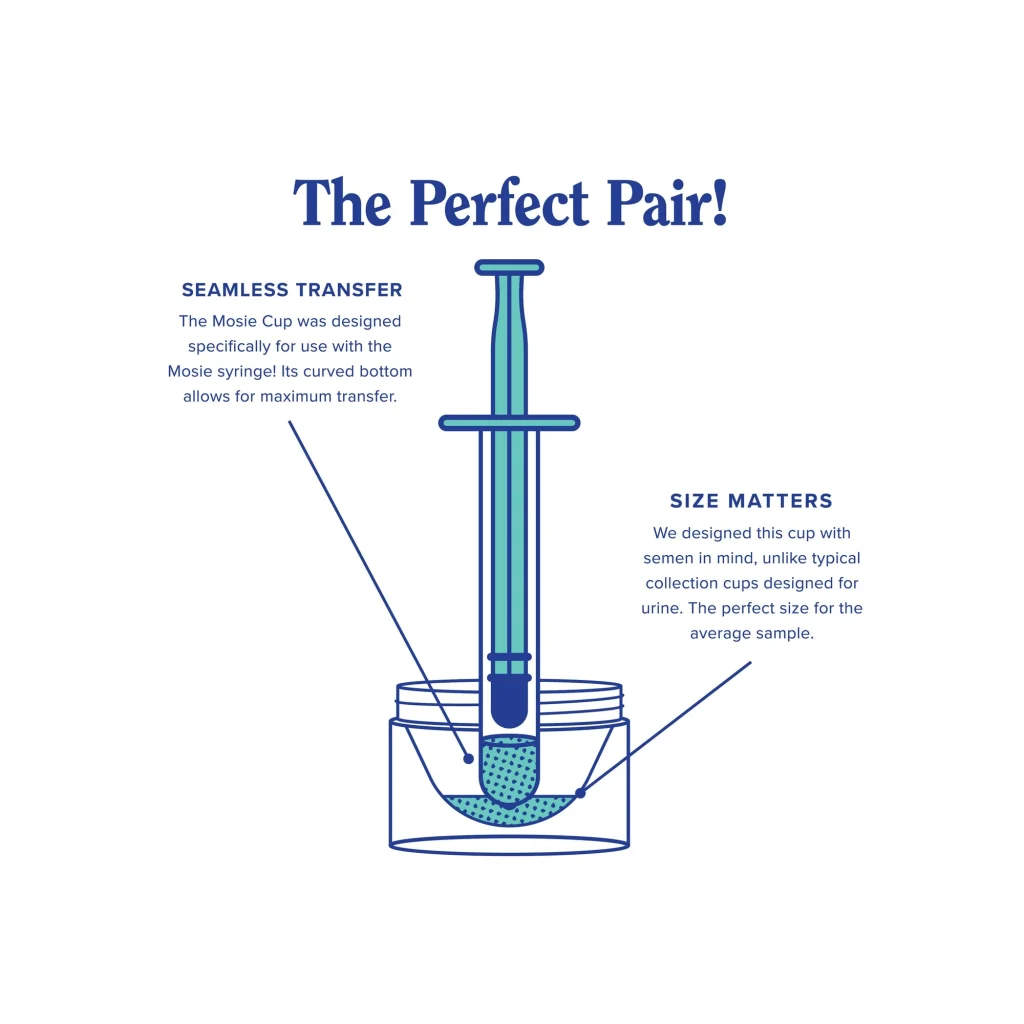
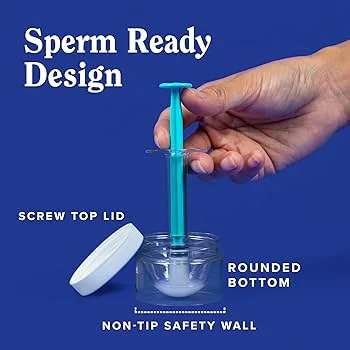
A home insemination kit for ICI is typically designed to help you collect and place sperm inside the vagina with less mess and more control. It is not the same as a clinic procedure, and it should not be used to attempt anything that goes through the cervix.
Look for clear labeling, simple components, and instructions that emphasize comfort and hygiene. If you have pelvic pain, a history of infections, or unexplained bleeding, check with a clinician before trying at home.
Relationship lens: How to avoid turning ICI into a monthly fight
At-home trying can feel “low stakes” until it isn’t. The emotional load often lands unevenly: one partner becomes the tracker, the scheduler, and the one who takes the physical discomfort. Resentment grows quietly when roles are assumed instead of chosen.
Try a two-minute reset after each attempt:
- Name the feeling: hopeful, numb, anxious, pressured.
- Name the need: space, reassurance, distraction, help with chores.
- Name the next step: what you will do before the next cycle.
It sounds small. It prevents big blowups.
Quick safety notes (non-clinical)
- Don’t improvise devices that aren’t intended for insemination.
- Don’t place anything through the cervix at home.
- Pause and seek medical care for fever, severe pain, foul odor, or heavy bleeding.
FAQs
Is ICI the same as IVF?
No. ICI is a low-tech method of placing sperm in the vagina, while IVF is lab fertilization with embryo transfer.
Can an at-home sperm donor become a legal parent?
In some jurisdictions, yes. Recent Florida reporting highlights that at-home arrangements can create legal openings depending on the facts. Get state-specific legal advice early.
What’s the difference between ICI and IUI?
IUI is usually performed in a clinic and places prepared sperm into the uterus. ICI is typically done at home and does not enter the uterus.
Do home insemination kits work?
They can, but outcomes vary widely based on timing and fertility factors. A clinician can help you decide when to escalate care.
What should we talk about before we try at home?
Consent, boundaries, finances, and what happens if it works or doesn’t. Add legal planning if a donor is involved.
CTA: Choose a kit, then choose a plan
If you’re leaning toward ICI, start with the basics: the right supplies, a clear timeline, and fewer misunderstandings. A purpose-built kit helps you stay consistent cycle to cycle.
How does at-home insemination (ICI) work?
Explore a at-home insemination kit for ICI and build a plan you can actually follow.
Medical disclaimer: This article is for general education and does not replace medical or legal advice. At-home insemination may not be appropriate for everyone. If you have health concerns, pain, unusual bleeding, or questions about fertility, consult a qualified clinician. For parentage and consent issues, consult a licensed attorney in your state.