Five rapid-fire takeaways before you decide:

- “35” is a loud number online, but fertility doesn’t flip like a switch on a birthday.
- At-home insemination (ICI) is about access and control, not “doing it perfectly.”
- Stress changes how you talk to each other; a plan can protect the relationship.
- Supplements are trending, but basics like timing, sperm health, and medical history still matter.
- Policy and court cases are in the news; if donors or parentage are involved, think ahead.
Why at-home ICI is everywhere right now
Between celebrity baby chatter, plotlines about surprise pregnancies in TV dramas, and constant “fertility cliff” debate, it can feel like everyone has an opinion about when and how to try. Headlines also keep circling women’s health, supplements, and reproductive rights litigation. That mix creates a cultural pressure cooker.
If you’re considering ICI, you’re not alone. Many people want a lower-intervention step before jumping to clinic care. Others want more privacy, more autonomy, or a calmer pace.
The decision guide: If…then… choose your next move
If you want a low-intervention first step, then ICI may fit
If you’re ovulating, cycles are fairly predictable, and there’s no known infertility diagnosis, ICI can be a reasonable home option to discuss. A home insemination kit is designed to help with clean, controlled placement and less mess. It can also reduce the “pressure performance” feeling that sometimes shows up with timed intercourse.
Relationship lens: agree on a short trial window (for example, a few cycles) so neither of you feels stuck in endless “maybe next month.”
If timing is causing arguments, then simplify the plan
If every cycle turns into a calendar negotiation, make the process smaller. Pick one tracking method you both trust, then set two planned attempts around the fertile window. Avoid daily re-litigating of symptoms and apps.
Some couples use tech to reduce mental load, the same way people lean on home insemination kit searches to understand tools that automate decisions. The goal is not to “optimize you.” It’s to protect your bandwidth.
If you’re thinking “We’re running out of time,” then zoom out from the number
The internet loves a single cutoff age, especially “35.” Recent conversations have pushed back on that idea, noting fertility depends on multiple factors for both partners. Age can matter, but it’s not the only variable, and it’s not a guaranteed cliff.
Try this reframe: instead of chasing a deadline, build a sequence. Home attempts first, then testing, then clinic options if needed. A sequence feels calmer than a countdown.
If donor sperm is involved, then plan for paperwork and peace of mind
When donor sperm enters the picture, the practical questions get bigger: consent, storage, shipping, and parentage. Since reproductive-health policy and court disputes are frequently in the headlines, it’s smart to clarify your local requirements and risk tolerance.
Tip for communication: decide together what “secure” means to you (clinic involvement, legal agreements, or both). Alignment now prevents resentment later.
If you suspect a medical factor, then consider testing sooner
If cycles are very irregular, you’ve had pelvic infections, endometriosis, recurrent pregnancy loss, or significant pain, don’t force yourself to “earn” medical support first. The same goes for known sperm concerns or prior chemotherapy/testicular injury.
Testing doesn’t commit you to IVF. It gives you information, which can make at-home tries more intentional.
If supplements are tempting, then treat them as optional—not the foundation
Supplement markets and “women’s health” roundups get a lot of attention. That can make it seem like the right capsule is the missing piece. In reality, supplements vary in quality, and they can interact with medications or conditions.
If you want to use them, consider running the list by a pharmacist or clinician. Keep your core plan focused on timing, safe handling, and realistic expectations.
How to keep ICI from taking over your relationship
Use a two-meeting rule: one short meeting to plan the cycle, one to debrief. Outside those meetings, you’re allowed to talk about anything else.
Name the invisible roles: one person often becomes the “project manager.” Swap tasks when possible. Even small changes help, like alternating who tracks ovulation vs who orders supplies.
Protect intimacy: schedule one no-baby-talk date per week. Pressure can flatten desire, and that’s nobody’s fault.
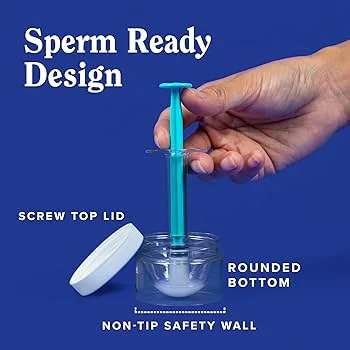
What to look for in a home insemination kit
- Comfort-focused design (smooth edges, easy grip, clear instructions).
- Hygiene and single-use components where appropriate.
- Clear labeling so you don’t improvise with items not meant for insemination.
- Support resources that explain ICI in plain language.
If you’re comparing options, start with a purpose-built product like an at-home insemination kit for ICI rather than DIY substitutes.
Medical disclaimer (please read)
This article is for general education and emotional support. It is not medical advice, and it cannot diagnose or treat any condition. If you have concerning symptoms (severe pain, heavy bleeding, fever), known fertility conditions, or questions about medications/supplements, consult a qualified clinician.
FAQs
Is ICI the same as IUI?
No. ICI places semen at or near the cervix, while IUI places washed sperm inside the uterus and is done in a clinic.
When is the best time to try ICI at home?
Many people aim for the fertile window around ovulation. If cycles are irregular or timing feels confusing, a clinician can help you choose a plan.
Can a home insemination kit help if we’re avoiding IVF?
It can be one lower-intervention option to try before moving to clinic-based treatments, depending on your situation and any known fertility factors.
Do fertility supplements replace medical care?
No. Supplements are widely marketed and actively discussed, but they don’t replace evaluation for ovulation issues, sperm concerns, or underlying health conditions.
When should we stop trying at home and get testing?
If you’ve been trying for months without progress, have very irregular cycles, known reproductive conditions, or significant pain/bleeding, it’s reasonable to ask for an evaluation sooner.
Is at-home insemination legal?
Rules vary by location and situation. If donor sperm, parentage, or custody could be an issue, consider legal guidance before you begin.
Next step: get a calmer, cleaner setup
If your goal is a private, lower-intervention attempt that still feels structured, start with a purpose-built home option and a shared plan for communication.