Decoding Cervical Mucus Changes for Reproductive Health: Understanding Your Body’s Signals
Cervical mucus may not be a topic that is commonly discussed, but it plays a crucial role in reproductive health. This sticky substance, produced by the cervix, is often referred to as the “fertility sign” as it changes throughout a woman’s menstrual cycle, indicating the best time for conception. Learning to decode these changes can not only help with family planning but also provide valuable insights into overall reproductive health.
What is Cervical Mucus?
Cervical mucus is a fluid secreted by the cervix, the lower part of the uterus that connects to the vagina. It is a mixture of water, proteins, enzymes, and electrolytes that serves multiple functions. One of the primary purposes of cervical mucus is to protect the reproductive organs from infections and foreign substances. It also provides lubrication during sexual intercourse and acts as a barrier, preventing sperm from entering the uterus except during the fertile window.
Cervical Mucus Changes Throughout the Menstrual Cycle
The menstrual cycle is a series of changes that occur in a woman’s body each month, preparing for a potential pregnancy. The cervical mucus goes through distinct changes during this cycle, which can be divided into four phases: the menstrual phase, the follicular phase, the ovulatory phase, and the luteal phase.
Menstrual Phase
During the menstrual phase, the cervix produces little to no mucus. This is because the body is shedding the lining of the uterus, and there is no need for cervical mucus to protect the reproductive organs.
Follicular Phase
The follicular phase begins after menstruation and lasts until ovulation. During this time, the body starts preparing for ovulation by producing estrogen, which stimulates the cervix to produce cervical mucus. The mucus is usually thick and sticky, and it creates a barrier, preventing sperm from entering the uterus.
Ovulatory Phase
The ovulatory phase is the most crucial phase for conception. During this time, the body releases an egg from the ovary, and the cervical mucus changes in response to the surge of estrogen. The mucus becomes thin, watery, and stretchy, resembling the consistency of egg whites. This fertile cervical mucus helps sperm travel through the cervix and into the uterus, increasing the chances of fertilization.
Luteal Phase
After ovulation, the body starts producing progesterone, which causes the cervical mucus to become thick and sticky again. This is to create a hostile environment for sperm, preventing them from reaching the uterus. If fertilization does not occur, the cervical mucus will dry up, and the cycle will repeat itself.
How to Decode Cervical Mucus Changes

Decoding Cervical Mucus Changes for Reproductive Health
Learning to recognize and interpret cervical mucus changes can be a valuable tool for family planning. Here are some tips for decoding cervical mucus changes:
1. Observe the Color and Consistency
Cervical mucus can vary in color and consistency, depending on the phase of the menstrual cycle. In the follicular phase, it is usually thick, cloudy, and sticky. During ovulation, it becomes thin, clear, and stretchy. In the luteal phase, it becomes thick, cloudy, and sticky again.
2. Check for Stretchiness
During ovulation, the cervical mucus becomes stretchy and can be stretched between the fingers without breaking. This is known as the “spinnbarkeit” effect and is a sign of fertile cervical mucus.
3. Monitor the Amount of Mucus
In the days leading up to ovulation, there is usually an increase in cervical mucus production. This can range from a few drops to a noticeable amount on underwear.
4. Keep Track of Changes in Basal Body Temperature
Basal body temperature (BBT) is the body’s temperature at rest. It tends to rise slightly after ovulation due to the increase in progesterone. Tracking BBT can help determine if ovulation has occurred and can confirm the changes in cervical mucus.
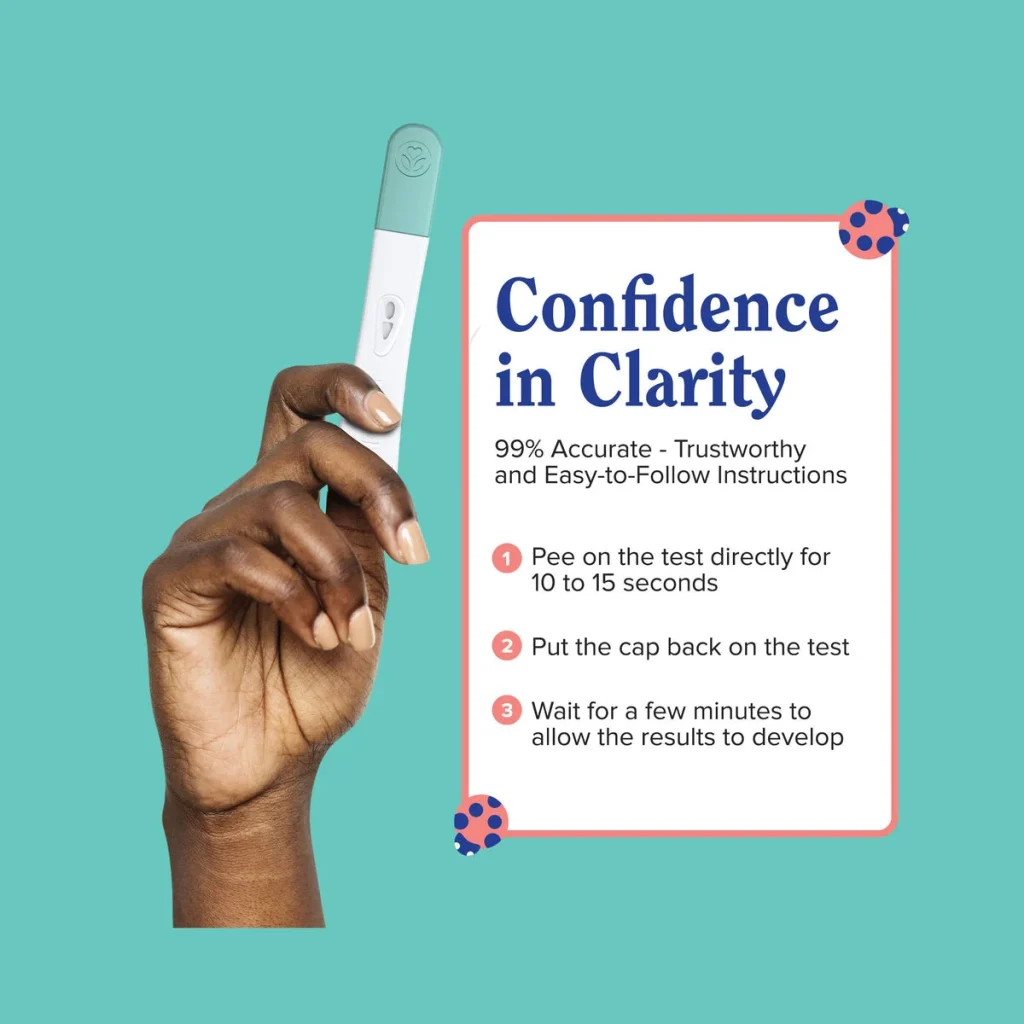
5. Use Ovulation Predictor Kits (OPKs)
OPKs are urine tests that detect the surge of luteinizing hormone (LH), which triggers ovulation. This surge usually occurs a day or two before ovulation, so using OPKs can help predict the fertile window.
Importance of Decoding Cervical Mucus Changes
Decoding cervical mucus changes is not only essential for family planning but also for overall reproductive health. Changes in cervical mucus can provide valuable insights into hormonal imbalances, infections, and other underlying health issues. For example, if the cervical mucus is consistently thick and sticky, it may indicate a lack of estrogen, which can affect fertility. On the other hand, if the cervical mucus is thin and watery throughout the cycle, it could be a sign of an infection or inflammation.
In conclusion, cervical mucus is a vital indicator of reproductive health, and learning to decode its changes can provide valuable information for family planning and overall well-being. By understanding the different phases of the menstrual cycle and observing the color, consistency, stretchiness, and amount of cervical mucus, women can gain a better understanding of their bodies and make informed decisions about their reproductive health.
Summary:
Cervical mucus is a fluid secreted by the cervix that changes throughout a woman’s menstrual cycle, indicating the best time for conception. It goes through four phases: menstrual, follicular, ovulatory, and luteal. By observing the color, consistency, stretchiness, and amount of cervical mucus, women can learn to decode its changes and use it as a tool for family planning and monitoring reproductive health. Changes in cervical mucus can also provide insights into hormonal imbalances and other health issues. Understanding the role of cervical mucus can empower women to take control of their reproductive health and make informed decisions.